Blog
Gastroshiza: Understanding Causes, Diagnosis, and Treatment

Introduction
Gastroshiza is a rare congenital defect where a baby is born with part of the intestines, and sometimes other abdominal organs, outside the body. Unlike similar conditions, gastroshiza has no protective sac around the exposed organs, which makes immediate medical attention necessary. Over the years, medical advances have drastically improved survival rates, and today most infants recover successfully with proper treatment.
This article explores gastroshiza in detail covering its causes, risk factors, symptoms, diagnostic methods, treatment strategies, and long-term outcomes.
What is Gastroshiza?
Gastroshiza, also called gastroschisis in medical literature, is a developmental condition that occurs early in pregnancy. Normally, the abdominal wall closes during fetal growth, enclosing the intestines. In gastroshiza, the wall fails to close completely, leaving an opening usually to the right of the umbilical cord through which the intestines protrude.
This condition differs from omphalocele, another abdominal wall defect, because the intestines in gastroshiza are not covered by a membrane. That absence increases the risk of irritation, infection, and fluid loss.
Causes and Risk Factors of Gastroshiza
The precise cause of gastroshiza is still uncertain. However, research has identified several contributing factors:
-
Maternal Age: Teen mothers under 20 have a higher chance of delivering babies with gastroshiza.
-
Environmental Exposure: Contact with pesticides, chemicals, or harmful substances during pregnancy may raise risks.
-
Lifestyle Choices: Smoking, alcohol, or recreational drug use during early pregnancy can contribute.
-
Nutrition: Lack of essential nutrients such as folic acid may play a role.
-
Genetics: Although not considered a hereditary condition, some genetic tendencies could influence development.
It’s important to note that most cases of gastroshiza occur randomly, without any family history.
Signs and Symptoms of Gastroshiza
The most obvious sign of gastroshiza is visible at birth: the baby’s intestines protruding through an opening near the belly button. Additional complications may include:
-
Swollen or inflamed intestines due to exposure to amniotic fluid.
-
Feeding difficulties because of impaired intestinal function.
-
Intestinal blockages or twisting.
-
Fluid and electrolyte imbalance.
Because gastroshiza is usually detected before birth, doctors can prepare for immediate care at delivery.
Diagnosis of Gastroshiza
Modern prenatal care allows doctors to identify gastroshiza before birth. Common diagnostic approaches include:
-
Ultrasound Scan – Around the 18th to 20th week of pregnancy, ultrasounds can reveal intestines outside the fetus’s abdominal wall.
-
Blood Tests – High levels of alpha-fetoprotein (AFP) in the mother’s blood may suggest an abdominal wall defect.
-
Postnatal Examination – If not caught prenatally, gastroshiza is immediately noticeable after delivery.
Early detection is crucial because it allows healthcare teams to plan for specialized neonatal and surgical support.
Treatment for Gastroshiza
Surgery is the only way to treat gastroshiza, and the approach depends on the severity of the defect.
Primary Closure Surgery
If the intestines are healthy and not too swollen, doctors may immediately place them back into the abdominal cavity and close the wall.
Staged Repair (Silo Technique)
When intestines are too swollen to fit at once, surgeons use a special sterile pouch called a “silo.” The intestines are gradually moved back inside over several days or weeks before the opening is closed.
Aftercare and Recovery
Following surgery, infants need:
-
IV nutrition until the intestines can process food.
-
Antibiotics to prevent infection.
-
Close monitoring for complications such as bowel obstruction or feeding issues.
Possible Complications
Although treatment success rates are high, gastroshiza can sometimes lead to complications such as:
-
Intestinal obstruction due to scarring or twisting.
-
Long-term feeding difficulties.
-
Infections from exposed intestines before surgery.
-
Prolonged hospitalization in neonatal intensive care units (NICU).
However, with modern neonatal care, most infants recover well and live healthy lives.
Prognosis and Outlook
Today, more than 90% of babies born with gastroshiza survive after proper treatment. Long-term outcomes are generally positive, especially when surgery is performed quickly and successfully. While some children may experience digestive issues in early years, most eventually catch up with normal growth and development.
Prevention and Maternal Care
There is no guaranteed way to prevent gastroshiza, but mothers can lower risks by:
-
Avoiding smoking, alcohol, and drugs during pregnancy.
-
Maintaining good nutrition and taking prenatal vitamins with folic acid.
-
Seeking regular prenatal checkups and ultrasounds.
-
Reducing exposure to harmful chemicals or toxins.
Public health awareness and early prenatal care are essential in reducing complications linked to gastroshiza.
Conclusion
Gastroshiza is a rare but serious birth defect requiring immediate medical care. Though its exact cause remains unclear, early detection, advanced surgical techniques, and specialized neonatal care have transformed the prognosis for affected infants. With timely intervention, most children born with gastroshiza grow up to live normal, healthy lives.
By raising awareness and encouraging expectant mothers to follow safe pregnancy practices, the chances of complications can be reduced, giving newborns the best possible start in life.
Blog
Popeye Jones Taylor Swift: Exploring the Surprising Connection Between Sports and Pop Culture
Blog
Texas Rangers vs Cincinnati Reds Match Player Stats: A Complete Performance Breakdown
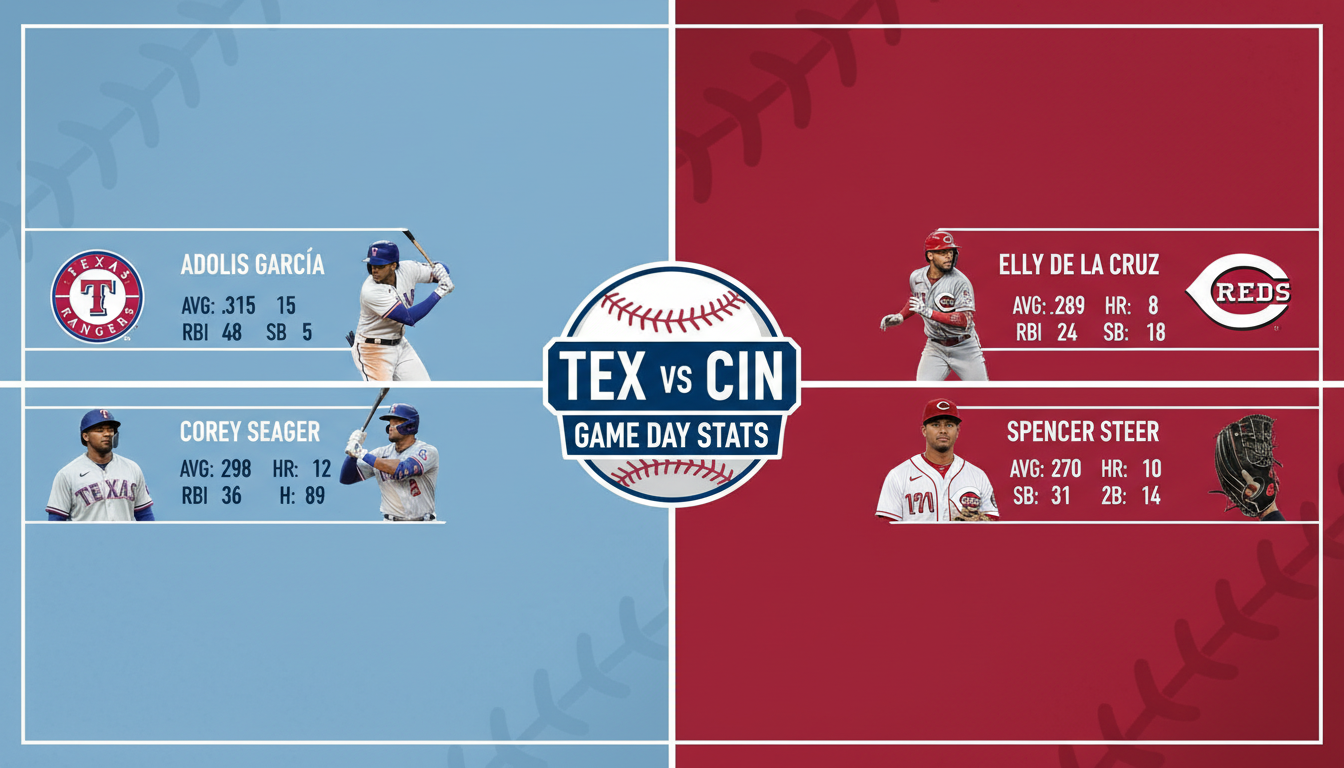
Baseball fans eagerly anticipate interleague clashes that bring together historic franchises with distinct playing styles. When the Texas Rangers face the Cincinnati Reds, attention quickly turns to performance metrics and individual contributions. Examining Texas Rangers vs Cincinnati Reds match player stats offers valuable insight into how each team executes its strategy on the field. From pitching accuracy to batting efficiency, every statistic tells part of the story. Understanding these numbers allows supporters and analysts to evaluate strengths, identify weaknesses, and appreciate the competitive balance that defines this compelling matchup.
Overview of Team Performance Dynamics
Analyzing Texas Rangers vs Cincinnati Reds match player stats begins with a broader look at overall team performance. The Rangers often emphasize offensive power, relying on consistent hitting and run production to gain momentum. Meanwhile, the Reds frequently focus on speed, defensive agility, and situational awareness. Comparing total runs, hits, errors, and on base percentages provides context for individual statistics. Team level data highlights how collective execution shapes outcomes. By examining these foundational metrics, observers can better interpret how standout performances contribute to the final score and overall competitive flow of the game.
Batting Leaders and Offensive Impact
Offensive production plays a central role in Texas Rangers vs Cincinnati Reds match player stats. Key hitters from both lineups influence scoring opportunities through batting averages, home runs, and runs batted in. A strong leadoff performance can set the tone, while middle order hitters often determine whether scoring chances are converted. Evaluating slugging percentage and on base plus slugging offers deeper insight into offensive efficiency. When players maintain disciplined plate approaches and capitalize on favorable pitches, their statistical contributions significantly shape the rhythm and momentum of the matchup.
Pitching Performance and Control Metrics
Pitching statistics are equally critical when reviewing Texas Rangers vs Cincinnati Reds match player stats. Starting pitchers establish early control through strike percentage, earned run average, and innings pitched. Relief pitchers then maintain or shift momentum depending on their command and composure under pressure. Strikeouts, walks allowed, and pitch velocity provide measurable indicators of effectiveness. A well executed pitching strategy can neutralize even the strongest batting lineup. By analyzing these metrics, fans gain a clearer understanding of how pitching depth and accuracy influence the overall balance of competition.
Defensive Contributions and Fielding Efficiency
Defense often determines close contests, making fielding data essential within Texas Rangers vs Cincinnati Reds match player stats. Fielding percentage, assists, and double plays reflect a team’s ability to prevent additional scoring. Quick reactions and accurate throws can halt potential rallies and shift momentum instantly. Outfield range and infield coordination also factor into limiting extra base hits. Strong defensive coordination supports pitchers and strengthens overall stability. Evaluating these statistics helps illustrate how disciplined defensive play complements offensive and pitching efforts throughout the course of the game.
Base Running and Speed Factors
Speed on the base paths adds another dimension to Texas Rangers vs Cincinnati Reds match player stats. Stolen bases, caught stealing attempts, and advancement on hits demonstrate how effectively players capitalize on opportunities. Aggressive yet calculated base running can pressure defensive units and create scoring openings. Teams that execute smart transitions between bases often gain subtle advantages. Tracking these numbers reveals which players consistently generate momentum through speed. Such contributions may not always appear dramatic, but they frequently influence tight outcomes in competitive matchups.
Key Player Matchups and Individual Rivalries
Individual matchups frequently shape the narrative of Texas Rangers vs Cincinnati Reds match player stats. When a dominant pitcher faces a power hitter, the statistical battle becomes particularly compelling. Historical head to head numbers can offer insight into how certain players perform against specific opponents. These micro contests within the broader game add strategic depth and excitement. Analyzing strikeout rates against particular batters or batting averages against certain pitchers highlights tactical adjustments. Such details enrich understanding of how personal performance trends affect overall team dynamics.
Advanced Analytics and Modern Metrics
Modern baseball analysis extends beyond traditional box score numbers. Advanced metrics play an increasing role in interpreting Texas Rangers vs Cincinnati Red match player stats. Statistics such as exit velocity, launch angle, and wins above replacement provide deeper insight into player value and efficiency. These measurements help evaluate consistency and long term impact rather than isolated results. By incorporating analytical data, teams refine strategies and optimize lineups. For fans, understanding these modern metrics enhances appreciation of the technical precision that defines contemporary baseball competition.
Impact of Coaching and Tactical Decisions
Coaching decisions significantly influence Texas Rangers vs Cincinnati Red match player stats. Strategic substitutions, bullpen management, and defensive alignments directly affect measurable outcomes. A timely pitching change can alter strikeout totals, while pinch hitters may shift offensive statistics late in the game. Managers analyze player data continuously to make informed adjustments. Tactical awareness ensures that individual performance aligns with broader team objectives. Evaluating these strategic factors alongside player statistics provides a more comprehensive understanding of how preparation and leadership shape competitive results.
What the Stats Reveal About Future Matchups
Reviewing Texas Rangers vs Cincinnati Red match player stats offers predictive value for future contests. Consistent performance patterns reveal strengths that teams may continue to exploit. Conversely, recurring weaknesses highlight areas requiring adjustment. Statistical trends guide coaching strategies, player development, and roster planning. By identifying which players consistently excel under specific conditions, analysts can anticipate potential advantages in upcoming games. This forward looking perspective demonstrates how detailed statistical analysis contributes not only to understanding past performances but also to shaping future competitive outcomes.
Conclusion
Texas Rangers vs Cincinnati Red match player stats provide a detailed window into the dynamics of this exciting baseball rivalry. From batting power and pitching precision to defensive skill and advanced analytics, each metric contributes to a comprehensive performance narrative. Careful examination of these statistics enhances appreciation for both individual talent and collective strategy. As teams continue to refine their approaches, statistical analysis remains central to understanding the evolving nature of the game. Through informed evaluation, fans gain deeper insight into the competitive spirit that defines every matchup.
Blog
The Importance of Expert Estimators in Achieving Accurate Project Cost Planning

Winning bids in today’s production marketplace callfor more than presenting the lowest quantity. It demands accuracy, strategy, and a deep know-how of substances, labor traits, and venture scope. Contractors who always secure worthwhile contracts understand that reliable value forecasting is the backbone of competitive bidding. Without professional estimating support, even the most promising projects can change into financially demanding situations.
Many contractors now collaborate with Construction Estimating Companies to strengthen their bidding process. These specialised corporations provide detailed amount takeoffs, cost analysis, and chance exams that help contractors submit practical and aggressive proposals. Instead of guessing or relying completely on experience, developers can approacheach sotaskith confidence supported by way of data-driven insights.
Why Accurate Estimating Determines Bid Success
In aggressive bidding environments, precision is the entirety. A bid that underestimates fabric prices with the aid of even a small margin can erode profits quickly. On the other hand, overestimating can also push your suggestion past a client’s financial budget. Professional estimators strike the proper balance by carefully comparing drawings, specs, and local marketplace situations.
For example, consider a business assignment valued at about $2 million. If material pricing fluctuates by way of 4% at some point of procurement and exertions productivity varies slightly from projections, the economic impact should reach tens of thousands of dollars. Professional estimators analyze such variables beforehand, decreasing uncertainty and defending your margins.
Accurate estimates additionally beautify credibility. Clients and builders select contractors who gift transparent, itemized breakdowns as opposed to rough lump-sum figures. Detailed documentation demonstrates professionalism and builds acceptance, growing your chances of being selected for repeat work.
Leveraging Detailed Plans for Cost Precision
Accurate estimating starts with nicely-organized drawings and technical documentation. This is where CAD Drafting Services play an essential role in the bidding method. Clear virtual drawings reduce ambiguity, allowing estimators to extract specific portions and perceive layout inconsistencies early.
For example, a small discrepancy in slab thickness throughout multiple floors may want to extensively regulate concrete volume calculations. When drafting and estimating work in coordination, such discrepancies are detected early, preventing high-priced bid mistakes. The result is an extra reliable idea that reflects actual venture necessities.
Additionally, up-to-date digital models allow quicker revisions whilst scope changes occur. During tender negotiations, clients often request changes. When drawings are without difficulty adjustable, estimators can directly replace quantities and pricing, assisting contractors in responding quickly and holding a competitive part.
Gaining a Competitive Edge Through Strategic Analysis
Competitive bidding isn’t certainly about numbers—it is approximately strategy. Professional estimators examine supplier rates, subcontractor pricing, and market trends to make sure bids continue to be both practical and appealing. They also consist of affordable contingencies to deal with capability risks without inflating the general idea.
Consider a situation in which metallic reinforcement charges boom by way of 6% due to market demand. A skilled estimator anticipates such trends and adjusts projections for that reason. This proactive method prevents unexpected value overruns at some stage in construction.
Furthermore, designated price breakdowns empower contractors to discover cost engineering options. If a project’s initial cost exceeds the customer’s budget, opportunity substances or production techniques can be proposed without compromising structural integrity. This flexibility complements your recognition as a solution-oriented contractor rather than without a doubt a bidder.
Improving Profit Margins Without Overpricing
One of the biggest misconceptions in bidding is that the lowest price wins. In truth, clients compare price, transparency, and reliability. Professional estimating help helps contractors optimize profit margins at the same time as remaining competitive.
Accurate takeoffs lessen cloth waste and over-ordering. For example, if a residential venture requires 15,000 square feet of drywall and the waste thing is cautiously calculated at 8%, ordering exactly the required amount prevents extra stock and pointless storage costs. Even minor improvements in procurement performance can undoubtedly impact standard profitability.
Additionally, specific labor forecasting improves scheduling performance. If a mission calls for three 000 exertions hours and productivity prices are appropriately assessed, venture managers can allocate workforce resources successfully. This reduces beyond regular time fees and maintains timelines on course—both important for maintaining profit margins.
Building Long-Term Business Growth Through Professional Support
Beyond character bids, steady estimating excellence contributes to long-term commercial enterprise growth. Contractors who publish accurate, profitable bids expand more potent purchaser relationships and steady repeat contracts. Over time, this consistency complements the lologo’seputation and market role.
Experienced Construction Estimators also assist contractors in analyzing historic data to refine destiny bidding techniques. By reviewing preceding undertaking consequences, businesses can identify traits in value variances and regulate forecasting models accordingly. This non-stop development process strengthens typical monetary stability.
Moreover, a professional estimating guide allows organization leadership to focus on operations and consumer engagement rather than spending excessive time preparing bids. Delegating complex price evaluation to specialists improves internal efficiency and ensures each proposal meets high professional standards.
Read More: How Much Does it Cost to Build a 2 Car Garage?
Final Thoughts
Hiring expert estimators is a strategic decision that directly affects your competitiveness and profitability. In an industry where margins are tight and competition is fierce, accurate cost forecasting affords the clarity needed to submit winning bids with self-belief.
From designated amount takeoffs to hazard evaluation and dealer coordination, expert estimating assistance enhances transparency and reduces monetary uncertainty. Contractors who invest in specific bidding techniques not only win extra projects,but also protect their bottom line. In the long term, partnering with professional estimating experts transforms bidding from anunstable gamble into a calculated approach for sustainable increase.
FAQs
- What contractors have to hire expert estimators for bidding?
Professional estimators offer correct cost breakdowns, helping contractors publish aggressive bids without risking income loss.
- How do correct estimates enhance profitability?
Precise forecasting prevents underpricing, reduces material waste, and ensures labor fees are realistically projected.
- Can expert estimating increase bid-triumphing chances?
Yes. Detailed and obvious proposals build patron agreement with and display professionalism, improving choice rates.
- Do estimators help manipulate marketplace rate fluctuations?
Absolutely. They reveal provider trends and include affordable contingencies to protect against surprising value increases.
- Is estimating aid useful for small contractors?
Yes. Even small construction corporations have a competitive advantage via correct, well-structured bids that enhance credibility and financial control.
Blog
Smart Material Calculation Methods for Reliable Project Budgeting
Accurate budgeting is the backbone of each hit creation challenge. Whether it’s a residential build, commercial improvement, or infrastructure work, the capability to forecast material demands precisely determines how smoothly the venture will continue. Poor calculations lead to delays, excess spending, garage issues, and, once in a while, compromised great. On the other hand, smart fabric making plans ensures that every aid is used effectively and each dollar is accounted for.
Modern creation is not predicated on tough estimates or guesswork. Today’s tasks demand records-driven decisions, specific analysis of plans, and coordinated procurement techniques. By applying the calculation methods early in the planning phase, project groups can reduce uncertainty and maintain financial control from start to finish.
The following sections explore verified techniques that help contractors, builders, and project managers gain reliable budgeting through specific fabric planning.
Accurate Wood Quantity Assessment for Structural Projects
Wood-framed production requires especially cautious planning because timber additives shape the structural spine of many residential and light commercial buildings. A detailed Lumber Takeoff affords a whole listing of required timber factors, which includes studs, beams, joists, rafters, sheathing, and connectors.
Accurate timber amount assessment begins with thoroughly reviewing architectural and structural drawings. Each factor has to be measured in line with distinctive dimensions, spacing requirements, and building codes. Even small miscalculations can multiply across large portions, leading to full-size price range discrepancies.
Precise calculations additionally assist determine premier slicing techniques. Standardizing lengths and minimizing offcuts reduces waste and lowers shopping charges. Additionally, knowing actual quantities allows bulk purchasing, which often results in better pricing from suppliers.
Minimizing Waste Through Optimized Material Planning
Material waste is one of the biggest hidden charges in construction. Excess ordering ties up capital and garage space, at the same time as shortages interrupt workflow and pressure pricey emergency purchases. Smart planning balances these dangers by way of aligning procurement with actual installation schedules.
Key waste-reduction strategies encompass:
- Phased shipping primarily based on creation development
- Standardized measurements to reduce trimming losses
- Careful garage making plans to prevent damage
- Coordination between trades to keep away from transform
Efficient fabric use no longer only saves money but additionally helps sustainability dreams. Reducing waste lowers environmental impact and improves an organisation’s reputation for accountable construction practices.
Data-Driven Forecasting for Financial Stability
Modern budgeting more and more relies on digital gear and ancient records. Software platforms can examine past projects, productivity rates, and market trends to produce quite accurate forecasts. These systems are replaced routinely while layout adjustments arise, making sure that cost projections remain current.
Benefits of information-pushed forecasting encompass:
- Early detection of financial risks
- Improved accuracy in comparison to manual calculations
- Faster assessment of design alternatives
- Greater transparency for buyers and customers
Reliable forecasts provide reassurance to all stakeholders. When monetary expectations are clear, selection-making will become more efficient, and disputes are much less likely to arise during creation.
Expertise That Transforms Plans into Actionable Costs
Even with advanced equipment, human knowledge remains crucial. A professional Construction estimator translates drawings, specifications, and site conditions to supply sensible value estimates. Their experience facilitates perceiving elements that a software program on my own might forget about, which include accessibility demanding situations, weather effects, or logistical constraints.
These professionals additionally compare constructability — determining whether or not the design can be constructed successfully the usage of to be had resources. They can also advise modifications that reduce fees without compromising structural integrity or capability.
Their position bridges the gap between theoretical plans and sensible execution. By translating complicated designs into clean monetary terms, they enable challenge groups to plan with a bit of luck and avoid expensive missteps.
Leveraging Technology for Precision and Efficiency
Technological innovation has transformed how fabric calculations are achieved. Tools that include Building Information Modeling (BIM), virtual plan analysis software, and cloud-based task structures enable enormously designated visualization and coordination.
Key technological blessings include:
- Automated amount extraction from 3-D models
- Detection of layout clashes earlier than creation
- Real-time updates across teams
- Improved documentation and responsibility
This equipment lessens human errors and accelerates planning strategies. They also allow teams to simulate one-of-a-kind situations, supporting them to perceive the maximum fee-powerful answers earlier than committing resources.
Professional Cost Evaluation for Budget Accuracy
While fabric quantities are crucial, accurate budgeting also depends on knowledge of marketplace fees, hard work charges, and device prices. Engaging expert Construction Estimating Services can notably decorate monetary making plans by way of presenting precise cost analysis based on contemporary enterprise information.
These experts review task drawings, specifications, and timelines to broaden comprehensive cost projections. They bear in mind variables which include local hard work costs, supplier pricing developments, transportation costs, and ability risks. This stage of detail permits stakeholders to put together practical budgets and keep away from unpleasant surprises later.
Read more: 10 Facts About Purple Heart Wood Characteristics and How It’s Used
Final Thoughts
Smart cloth calculation methods are essential for reliable mission budgeting in today’s production environment. Accurate amount tests, expert price analysis, expert interpretation, and collaborative planning all make contributions to financial stability and a hit project shipping.
Rather than reacting to problems throughout production, forward-thinking groups spend money on thorough instruction. This proactive approach minimizes waste, prevents delays, and ensures that resources are used efficaciously. In a competitive industry in which margins are often tight, unique planning can make the distinction between earnings and losses.
Ultimately, the most successful tasks are those that start with clarity, accuracy, and coordination. By embracing modern calculation strategies and strategic planning practices, developers can deliver extremely good consequences at the same time as keeping strict price range control.
Frequently Asked Questions (FAQs)
- Why is correct fabric calculation important in creation?
It guarantees that the right quantities are ordered, stopping
- How can tasks lessen cloth waste?
Through specific planning, phased deliveries, standardized measurements, and the right garage to save you harm.
- Do small tasks need professional value analysis?
Yes. Even smaller builds can benefit from professional insights to avoid hidden expenses and ensure practical budgeting.
- How does technology improve budgeting accuracy?
Digital gear automates calculations, analyzes ancient facts, and replaces charges in actual time as changes arise.
Blog
MyUTRGV: A Complete Guide to the University of Texas Rio Grande Valley Student Portal
Blog
Fotosista: Understanding the Role and Importance of a Modern Photosynthesis Specialist
Blog
The Power of Straightforward Talk: Building Trust Through Clear Communication
Blog
Irish Business Systems: Driving Efficiency and Digital Growth in Modern Enterprises
-
 Entertainment5 months ago
Entertainment5 months agoOGFap Review: Pros, Cons, and User Experience
-

 Fashion4 months ago
Fashion4 months agoComme des Garcons: The Iconic Avant-Garde Fashion Brand
-

 Blog5 months ago
Blog5 months agoi̇ns: Exploring Its Meaning, Values, and Modern Impact
-

 Blog5 months ago
Blog5 months ago鲁Q 669FD License Plate Lookup – Car History & Vehicle Records
-

 Uncategorized5 months ago
Uncategorized5 months agoManga18fz: A Complete Guide to the Trending Manga Platform
-

 Fashion4 months ago
Fashion4 months agoCustom Jersey Printing: Designing Your Team’s Identity with SeamJersey
-

 Blog4 months ago
Blog4 months agoRuisseau d’Avenelle: A Peaceful Escape into Nature
-

 Technology6 months ago
Technology6 months agoSimpcit6: Unlocking the Next Phase of Digital Simplicity






